| Revision as of 20:53, 4 March 2012 editBuster23 (talk | contribs)Extended confirmed users697 edits Difficulty in defining a disease versus a syndrome← Previous edit | Revision as of 20:58, 4 March 2012 edit undoBuster23 (talk | contribs)Extended confirmed users697 edits Link to wikipedia page on disease rather than add full explanation here.Next edit → | ||
| Line 10: | Line 10: | ||
| PANDAS is hypothesized to be an ] that results in a variable combination of tics, obsessions, compulsions, and other symptoms that may be severe enough to qualify for diagnoses such as chronic tic disorder, OCD, and Tourette's. The cause is thought to be akin to that of ], which is known to result from childhood ] leading to the autoimmune disorder ] of which Sydenham's is one manifestation. Like Sydenham's, PANDAS is thought to involve autoimmunity to the brain's ]. Unlike Sydenham's, PANDAS is not associated with other manifestations of acute rheumatic fever, such as ].<ref name=Pichichero2009>{{Cite journal|author=Pichichero ME |title=The PANDAS syndrome |journal=Adv Exp Med Biol |volume=634 |pages=205–16 |year=2009 |pmid=19280860 | url=http://books.google.com/?id=CxfTmEAqdAoC&lpg=PR2&pg=PA205#v=onepage&q=pichichero |publisher=Springer |isbn=9780387798370|doi=10.1007/978-0-387-79838-7_17|series=Advances in Experimental Medicine and Biology }}</ref> | PANDAS is hypothesized to be an ] that results in a variable combination of tics, obsessions, compulsions, and other symptoms that may be severe enough to qualify for diagnoses such as chronic tic disorder, OCD, and Tourette's. The cause is thought to be akin to that of ], which is known to result from childhood ] leading to the autoimmune disorder ] of which Sydenham's is one manifestation. Like Sydenham's, PANDAS is thought to involve autoimmunity to the brain's ]. Unlike Sydenham's, PANDAS is not associated with other manifestations of acute rheumatic fever, such as ].<ref name=Pichichero2009>{{Cite journal|author=Pichichero ME |title=The PANDAS syndrome |journal=Adv Exp Med Biol |volume=634 |pages=205–16 |year=2009 |pmid=19280860 | url=http://books.google.com/?id=CxfTmEAqdAoC&lpg=PR2&pg=PA205#v=onepage&q=pichichero |publisher=Springer |isbn=9780387798370|doi=10.1007/978-0-387-79838-7_17|series=Advances in Experimental Medicine and Biology }}</ref> | ||
| To be classified as a disease, a disorder must show that |
To be classified as a ], a disorder must show that a particular part of the body is affected or that the symptoms occur if and only if the trigger or cause occurs. PANDAS has not been validated as a disease classification, for several reasons. Its proposed age of onset and clinical features reflect a particular group of patients chosen for research studies, with no systematic studies of the possible relationship of GAS to other neurologic symptoms. There is controversy over whether its symptom of choreiform movements is distinct from the similar movements of Sydenham's. It is not known whether the pattern of abrupt onset is specific to PANDAS. Finally, there is controversy over whether there is a temporal relationship between GAS infections and PANDAS symptoms.<ref name=Pichichero2009/> | ||
| Given the controversy on the etiology of PANDAS (i.e., whether caused by strep throat) and the apparent ambiguity in the definitions of the clinical presentation leading to different research results, a new definition was proposed that would clarify the presentation of symptoms to ensure that research studies were studying the same group of children. <ref name=Swedo2012 /> This proposed syndrome is called ](PANS). PANS, removes the requirement of temporal association with strep throat and adds the "abrupt, dramatic onset of ] (OCD) or severely restricted food intake" coincident with the presence of two or more neuropsychiatric symptoms.<ref name=Swedo2012>{{Cite journal |author= Swedo SE, Leckman JF, Rose NR |title= From research subgroup to clinical syndrome: modifying the PANDAS criteria to describe PANS (Pediatric acute-onset neuropsychiatric syndrome)|journal=Pediatr Therapeut. |year= 2012 |month= Feb |volume=2|issue= 2 | url=http://pandasnetwork.org/wp-content/uploads/2012/02/2161-0665-2-113.pdf | format=PDF |doi=10.4172/2161-0665.1000113}}</ref> The proposed syndrome definition comes from a decade of comparative studies on the PANDAS hypothesis and argues that the severity, abruptness and dramatic onset of symptoms differentiates the children from traditional childhood OCD.<ref name=Swedo2012/> | Given the controversy on the etiology of PANDAS (i.e., whether caused by strep throat) and the apparent ambiguity in the definitions of the clinical presentation leading to different research results, a new definition was proposed that would clarify the presentation of symptoms to ensure that research studies were studying the same group of children. <ref name=Swedo2012 /> This proposed syndrome is called ](PANS). PANS, removes the requirement of temporal association with strep throat and adds the "abrupt, dramatic onset of ] (OCD) or severely restricted food intake" coincident with the presence of two or more neuropsychiatric symptoms.<ref name=Swedo2012>{{Cite journal |author= Swedo SE, Leckman JF, Rose NR |title= From research subgroup to clinical syndrome: modifying the PANDAS criteria to describe PANS (Pediatric acute-onset neuropsychiatric syndrome)|journal=Pediatr Therapeut. |year= 2012 |month= Feb |volume=2|issue= 2 | url=http://pandasnetwork.org/wp-content/uploads/2012/02/2161-0665-2-113.pdf | format=PDF |doi=10.4172/2161-0665.1000113}}</ref> The proposed syndrome definition comes from a decade of comparative studies on the PANDAS hypothesis and argues that the severity, abruptness and dramatic onset of symptoms differentiates the children from traditional childhood OCD.<ref name=Swedo2012/> | ||
Revision as of 20:58, 4 March 2012
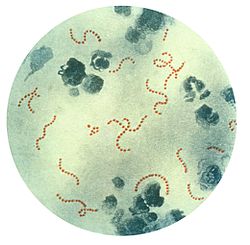
PANDAS is an acronym for Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections. This term describes a hypothesis that there exists a subset of children with rapid onset of obsessive-compulsive disorder (OCD) and/or tic disorders and these symptoms are caused by group A beta-hemolytic streptococcal (GABHS) infections such as "strep throat" and scarlet fever. The proposed link between infection and these disorders is an autoimmune reaction, where antibodies produced to the infection interfere with neuronal cells.
The PANDAS hypothesis is based on observations in clinical case studies at the National Institute of Health and in subsequent clincial trials where children matching a particular profile appeared to have dramatic and sudden OCD exacerbations and tic disorders following infections. The attractiveness of the hypothesis is that if true, new avenues of treatment and prevention might be available. The concern regarding the hypothesis is that if false, these patients may be improperly treated. Although there is evidence linking infection and onset in some OCD/tic cases, proving a true causal relationship has remained elusive. The PANDAS hypothesis is controversial and its usefulness is disputed by some scientists who think these patients do not differ significantly from the remainder of the patient population, and that infections do not increase the risk of OCD or tics. Consequently, the PANDAS model is a complex and rapidly-moving area of medical research. PANDAS is not listed as a diagnosis by the International Statistical Classification of Diseases and Related Health Problems (ICD) or the Diagnostic and Statistical Manual of Mental Disorders (DSM).
Pediatric acute-onset neuropsychiatric syndrome (PANS) is a newer hypothesis used to describe a subset of acute-onset OCD cases; the newer hypothesis includes "all cases of abrupt onset OCD, not just those associated with streptococcal infections".
Classification

PANDAS is hypothesized to be an autoimmune disorder that results in a variable combination of tics, obsessions, compulsions, and other symptoms that may be severe enough to qualify for diagnoses such as chronic tic disorder, OCD, and Tourette's. The cause is thought to be akin to that of Sydenham's chorea, which is known to result from childhood Group A streptococcal (GAS) infection leading to the autoimmune disorder acute rheumatic fever of which Sydenham's is one manifestation. Like Sydenham's, PANDAS is thought to involve autoimmunity to the brain's basal ganglia. Unlike Sydenham's, PANDAS is not associated with other manifestations of acute rheumatic fever, such as inflammation of the heart.
To be classified as a disease, a disorder must show that a particular part of the body is affected or that the symptoms occur if and only if the trigger or cause occurs. PANDAS has not been validated as a disease classification, for several reasons. Its proposed age of onset and clinical features reflect a particular group of patients chosen for research studies, with no systematic studies of the possible relationship of GAS to other neurologic symptoms. There is controversy over whether its symptom of choreiform movements is distinct from the similar movements of Sydenham's. It is not known whether the pattern of abrupt onset is specific to PANDAS. Finally, there is controversy over whether there is a temporal relationship between GAS infections and PANDAS symptoms.
Given the controversy on the etiology of PANDAS (i.e., whether caused by strep throat) and the apparent ambiguity in the definitions of the clinical presentation leading to different research results, a new definition was proposed that would clarify the presentation of symptoms to ensure that research studies were studying the same group of children. This proposed syndrome is called Pediatric Acute-onset Neuropsychiatric Syndrome(PANS). PANS, removes the requirement of temporal association with strep throat and adds the "abrupt, dramatic onset of obsessive-compulsive disorder (OCD) or severely restricted food intake" coincident with the presence of two or more neuropsychiatric symptoms. The proposed syndrome definition comes from a decade of comparative studies on the PANDAS hypothesis and argues that the severity, abruptness and dramatic onset of symptoms differentiates the children from traditional childhood OCD.
Identification
According to the National Institute of Mental Health (NIMH), children with symptoms of PANDAS are clinically identified by five criteria:
- Existence of obsessive-compulsive disorder or a tic disorder.
- Abrupt symptom onset with an episodic (relapsing/remitting) course of symptom severity.
- Onset before puberty.
- May include other neuropsychiatric symptoms (with similarly abrupt onset).
- Associated with Group A Beta Hemolytic Stretococcal infection.
The children usually have dramatic, "overnight" onset of symptoms, including motor or vocal tics, obsessions, and/or compulsions. Some studies have shown no acute exacerbations associated with streptococcal infections among clinically defined PANDAS subjects whilst others have shown a profound one.
In addition to an OCD or tic disorder diagnosis, children may have other symptoms associated with exacerbations such as emotional lability, enuresis, anxiety, and deterioration in handwriting. In the PANDAS model, this abrupt onset is thought to be preceded by a strep throat infection. As the clinical spectrum of PANDAS appears to resemble that of Tourette's syndrome, some researchers hypothesized that PANDAS and Tourette's may be associated; this idea is controversial and a focus for current research.
Concerns have been raised that PANDAS may be overdiagnosed, as a significant number of patients diagnosed with PANDAS by community physicians did not meet the criteria when examined by specialists, suggesting that the PANDAS diagnosis is conferred by community physicians without conclusive evidence.
Proposed mechanism
The PANDAS diagnosis and the hypothesis that symptoms in this subgroup of patients are caused by infection are controversial.
Whether the group of patients diagnosed with PANDAS have developed tics and OCD through a different mechanism (pathophysiology) than seen in other people diagnosed with Tourette syndrome is unclear. Researchers are pursuing a hypothesis that the mechanism is similar to that of rheumatic fever, an autoimmune disorder triggered by streptococcal infections, where antibodies attack the brain and cause neuropsychiatric conditions.
In a typical bacterial infection, the body produces antibodies against the invading bacteria, and the antibodies help eliminate the bacteria from the body. However in rheumatic fever, the antibodies mistakenly recognize and "attack" the heart valves, joints, and/or certain parts of the brain. This phenomenon is called "molecular mimicry", which means that antigens on the cell wall of the streptococcal bacteria are similar in some way to the proteins of the heart valve, joints, or brain. Because the antibodies set off an immune reaction which damages those tissues, the child with rheumatic fever can get heart disease (especially mitral valve regurgitation), arthritis, and/or abnormal movements known as Sydenham's chorea or "St. Vitus' Dance". In PANDAS, it is believed that tics and OCD are produced in a similar manner. One part of the brain that may be affected in PANDAS is the basal ganglia, which is believed to be responsible for movement and behavior. It is thought that similar to Sydenham's chorea, the antibodies cross-react with neuronal brain tissue in the basal ganglia to cause the tics and OCD that characterize PANDAS. However, current data neither disprove nor support this hypothesis, indeed one recent study found no association between treated streptococcal infections and the risk of PANDAS symptoms.
Experimental treatments
Prophylactic antibiotic treatments for tics and OCD are experimental and controversial; overdiagnosis of PANDAS may have led to overuse of antibiotics to treat tics or OCD in the absence of active infection. An initial study with 37 children found no effect of prophylactic antibiotic treatment on either infection rate or obsessive-compulsive or tic symptom severity, a second study on 23 children later suggested that antibiotics were beneficial. However, the methods in both studies have been criticized.
A single study of PANDAS patients showed efficacy of immunomodulatory therapy to symptoms, but these results are unreplicated by independent studies as of 2010. According to the NIMH and the Advisory Board of the Tourette Syndrome Association, experimental treatments based on the autoimmune theory such as intravenous immunoglobulin (IVIG) or plasma exchange should be "reserved for severely ill patients" and should not be undertaken outside of formal clinical trials.
Pediatric acute-onset neuropsychiatric syndrome
Pediatric acute-onset Neuropschiatric Syndrome is a proposal of a research criteria to assist scientists and clinicians to compare similar children across studies. The new criteria focuses solely on the clinical presentation and not on the cause or etiology. The proposed criteria claims that children can be distinguished from traditional childhood onset OCD by the severity, abruptness and dramatic onset of symptoms.
Children and adolescents hypothesized to have PANS would be identified by the following three criteria:
- Abrupt, dramatic onset of obsessive-compulsive disorder or severely restricted food intake
- Concurrent presence of additional neuropsychiatric symptoms, with similarly severe and acute onset, from at least two of the following seven categories
- Anxiety
- Emotional lability and/or depression
- Irritability, aggression and/or severely oppositional behaviors
- Behavioral (developmental) regression
- Deterioration in school performance
- Sensory or motor abnormalities
- Somatic signs and symptoms, including sleep disturbances, enuresis or urinary frequency
- Symptoms are not better explained by a known neurologic or medical disorder, such as Sydenham's chorea, systemic lupus erythematosus, Tourette disorder or others.
There are other conditions that may have similar presentation; diagnostic workup of individuals suspected of PANS should exclude Sydenham's chorea, lupus erythematosus, acute disseminated encephalomyelitis, and Tourette syndrome. Evidence of acute rheumatic fever would exclude a PANS classification. Depending on neuropsychiatric symptoms, diagnostic tests may include magnetic resonance imaging (MRI), lumbar puncture, and electroencephalography (EEG).
See also
References
- ^ NIH. PANDAS. Retrieved 24 February 2012.
- Kirvan CA, Swedo SE, Kurahara D, Cunningham MW (2006). "Streptococcal mimicry and antibody-mediated cell signaling in the pathogenesis of Sydenham's chorea". Autoimmunity. 39 (1): 21–9. doi:10.1080/08916930500484757. PMID 16455579.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pichichero ME (2009). "The PANDAS syndrome". Adv Exp Med Biol. Advances in Experimental Medicine and Biology. 634. Springer: 205–16. doi:10.1007/978-0-387-79838-7_17. ISBN 9780387798370. PMID 19280860.
- ^ Shulman ST (2009). "Pediatric autoimmune neuropsychiatric disorders associated with streptococci (PANDAS): update". Curr. Opin. Pediatr. 21 (1): 127–30. doi:10.1097/MOP.0b013e32831db2c4. PMID 19242249.
{{cite journal}}: Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help); Unknown parameter|month=ignored (help) - ^ Shulman ST (2009). "Pediatric autoimmune neuropsychiatric disorders associated with streptococci (PANDAS): update". Curr. Opin. Pediatr. 21 (1): 127–30. doi:10.1097/MOP.0b013e32831db2c4. PMID 19242249.
Despite continued research in the field, the relationship between GAS and specific neuropsychiatric disorders (PANDAS) remains elusive.
{{cite journal}}: Unknown parameter|month=ignored (help) - Maia TV, Cooney RE, Peterson BS (2008). "The neural bases of obsessive-compulsive disorder in children and adults". Dev. Psychopathol. 20 (4): 1251–83. doi:10.1017/S0954579408000606. PMC 3079445. PMID 18838041.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Singer HS, Williams PN (2006). "Autoimmunity and pediatric movement disorders". Adv Neurol. 99: 166–78. PMID 16536363.
- Leckman JF, Bloch MH, King RA (2009). "Symptom dimensions and subtypes of obsessive–compulsive disorder: a developmental perspective" (PDF). Dialogues Clin Neurosci. 11 (1): 21–33. PMC 3181902. PMID 19432385.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Lombroso PJ, Scahill L (2008). "Tourette syndrome and obsessive–compulsive disorder". Brain Dev. 30 (4): 231–7. doi:10.1016/j.braindev.2007.09.001. PMC 2291145. PMID 17937978.
- ^ Swedo SE, Leckman JF, Rose NR (2012). "From research subgroup to clinical syndrome: modifying the PANDAS criteria to describe PANS (Pediatric acute-onset neuropsychiatric syndrome)" (PDF). Pediatr Therapeut. 2 (2). doi:10.4172/2161-0665.1000113.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) Cite error: The named reference "Swedo2012" was defined multiple times with different content (see the help page). - ^ Luo F, Leckman J, Katsovich L; et al. (2004). "Prospective longitudinal study of children with tic disorders and/or obsessive-compulsive disorder: relationship of symptom exacerbations to newly acquired streptococcal infections". Pediatrics. 113 (6): e578–85. doi:10.1542/peds.113.6.e578. PMID 15173540.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Singer HS, Hong JJ, Yoon DY, Williams PN (2005). "Serum autoantibodies do not differentiate PANDAS and Tourette syndrome from controls". Neurology. 65 (11): 1701–7. doi:10.1212/01.wnl.0000183223.69946.f1. PMID 16207842.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Loiselle CR, Wendlandt JT, Rohde CA, Singer HS (2003). "Antistreptococcal, neuronal, and nuclear antibodies in Tourette syndrome". Pediatr. Neurol. 28 (2): 119–25. doi:10.1016/S0887-8994(02)00507-6. PMID 12699862.{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Loiselle CR, Lee O, Moran TH, Singer HS (2004). "Striatal microinfusion of Tourette syndrome and PANDAS sera: failure to induce behavioral changes". Mov. Disord. 19 (4): 390–6. doi:10.1002/mds.10522. PMID 15077236.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Murphy TK, Sajid M, Soto O, ; et al. (2004). "Detecting pediatric autoimmune neuropsychiatric disorders associated with streptococcus in children with obsessive-compulsive disorder and tics". Biol Psychiatry. 55 (1): 61–8. doi:10.1016/S0006-3223(03)00704-2. PMID 14706426.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Moretti G, Pasquini M, Mandarelli G, Tarsitani L, Biondi M (2008). "What every psychiatrist should know about PANDAS: a review". Clin Pract Epidemol Ment Health. 4 (1): 13. doi:10.1186/1745-0179-4-13. PMC 2413218. PMID 18495013.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Singer HS (2005). "Tourette's syndrome: from behaviour to biology". Lancet Neurol. 4 (3): 149–59. doi:10.1016/S1474-4422(05)01012-4. PMID 15721825.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Leckman JF, Denys D, Simpson HB; et al. (2010). "Obsessive-compulsive disorder: a review of the diagnostic criteria and possible subtypes and dimensional specifiers for DSM-V" (PDF). Depress Anxiety. 27 (6): 507–27. doi:10.1002/da.20669. PMID 20217853.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Singer HS, Loiselle C (2003). "PANDAS: a commentary". J Psychosom Res. 55 (1): 31–9. doi:10.1016/S0022-3999(02)00582-2. PMID 12842229.
{{cite journal}}: Unknown parameter|month=ignored (help) - Kurlan R, Kaplan EL (2004). "The pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection (PANDAS) etiology for tics and obsessive–compulsive symptoms: hypothesis or entity? Practical considerations for the clinician" (PDF). Pediatrics. 113 (4): 883–86. doi:10.1542/peds.113.4.883. PMID 15060240.
{{cite journal}}: Unknown parameter|month=ignored (help) - Dale RC (2005). "Post-streptococcal autoimmune disorders of the central nervous system". Dev Med Child Neurol. 47 (11): 785–91. doi:10.1017/S0012162205001647. PMID 16225745.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Swedo S (2002). "Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS)" (PDF). Mol Psychiatry. 7. Suppl 2 (s2): S24–5. doi:10.1038/sj.mp.4001170. PMID 12142939.
- Rullan E, Sigal L (2001). "Rheumatic fever". Curr Rheumatol Rep. 3 (5): 445–52. doi:10.1007/s11926-996-0016-4. PMID 11564377.
- Bonthius D, Karacay B (2003). "Sydenham's chorea: not gone and not forgotten". Semin Pediatr Neurol. 10 (1): 11–9. doi:10.1016/S1071-9091(02)00004-9. PMID 12785743.
- Perrin E, Murphy M, Casey J; et al. (2004). "Does group A beta-hemolytic streptococcal infection increase risk for behavioral and neuropsychiatric symptoms in children?". Arch Pediatr Adolesc Med. 158 (9): 848–56. doi:10.1001/archpedi.158.9.848. PMID 15351749.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Garvey M, Perlmutter S, Allen A, et a; (1999). "A pilot study of penicillin prophylaxis for neuropsychiatric exacerbations triggered by streptococcal infections". Biol Psychiatry. 45 (12): 1564–71. doi:10.1016/S0006-3223(99)00020-7. PMID 10376116.
{{cite journal}}: CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - Snider L, Lougee L, Slattery M, Grant P, Swedo S (2005). "Antibiotic prophylaxis with azithromycin or penicillin for childhood-onset neuropsychiatric disorders". Biol Psychiatry. 57 (7): 788–92. doi:10.1016/j.biopsych.2004.12.035. PMID 15820236.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Gilbert D, Gerber M (2005). "Regarding "antibiotic prophylaxis with azithromycin or penicillin for childhood-onset neuropsychiatric disorders"". Biol Psychiatry. 58 (11): 916. doi:10.1016/j.biopsych.2005.08.004. PMID 16242119.
- Scahill L, Erenberg G, Berlin CM; et al. (2006). "Contemporary assessment and pharmacotherapy of Tourette syndrome" (PDF). NeuroRx. 3 (2): 192–206. doi:10.1016/j.nurx.2006.01.009. PMID 16554257.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
External links
| Tourette syndrome | |
|---|---|
| Main | |
| Terms | |
| Assessment tools | |
| People | |
| Organizations | |
| Media | |
Categories: